A dental implant is an artificial tooth root that is placed into your jaw to hold a replacement tooth or bridge. Dental implants are an ideal option for people in good general oral health who have lost a tooth or teeth due to periodontal disease, an injury, or some other reason. Dental implants look and feel like natural teeth, and with proper care, they can be a long-term solution to tooth replacement.
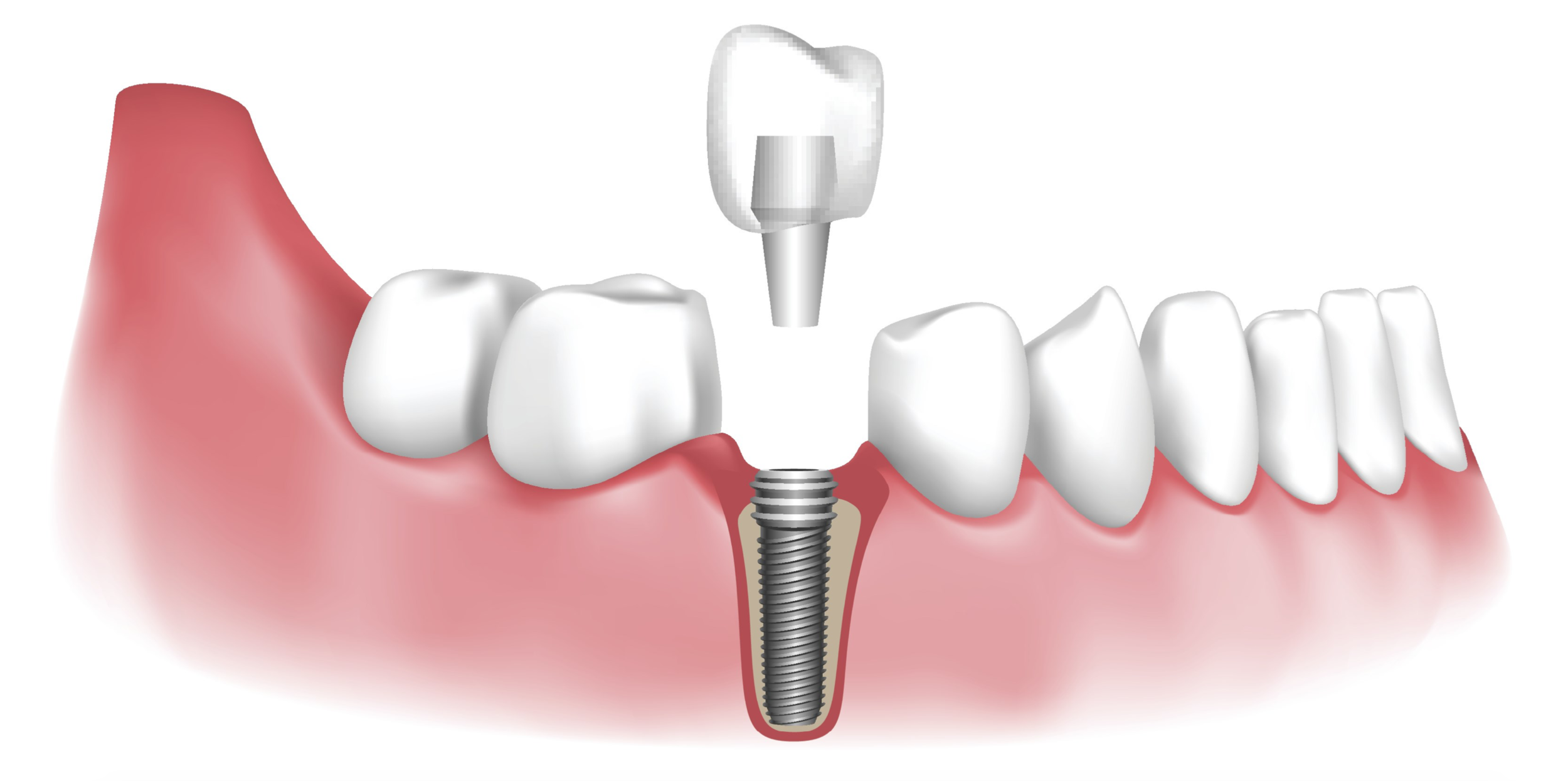
The procedure involves a titanium screw/post, which is surgically placed into your jaw. Over the next few months, the implant and bone are then allowed to bond together to form an anchor for your artificial teeth. During this time, a temporary tooth replacement option can be worn. Sometimes a second procedure is needed to place an extension on the implant. This small metal post, called an abutment, completes the foundation on which your new tooth will be placed. The replacement tooth (or bridge or denture) will then be created by your general dental professional and attached to the implant.
Dental implants look and function like natural teeth, and they require the same care. We recommend brushing twice a day, flossing at least once a day, and receiving regular check-ups including an annual comprehensive periodontal evaluation.
Additional procedures may be required before an implant can be placed:
“Bone Grafting” or “Ridge Modification” may be needed if you don’t have enough bone to support an implant. During this procedure, bone or bone substitute is added where needed to ensure a proper foundation for implants.
“Sinus augmentation” may be needed to place implants in the upper back jaw, where your bone is very close to your sinus. In this procedure, the sinus floor is raised so there is more room for new bone to grow to provide a proper foundation for implants.
“Gum Grafting” may be necessary to improve the quantity or quality of tissues for a future dental implant.
All of these procedures have been shown to greatly increase your chances for successful implants that can last for years to come.